⭐⭐ PARAPLEGIA ⭐⭐
⭐⭐ PARAPLEGIA ⭐⭐
1) DEFINITION OF PARAPLEGIA :-
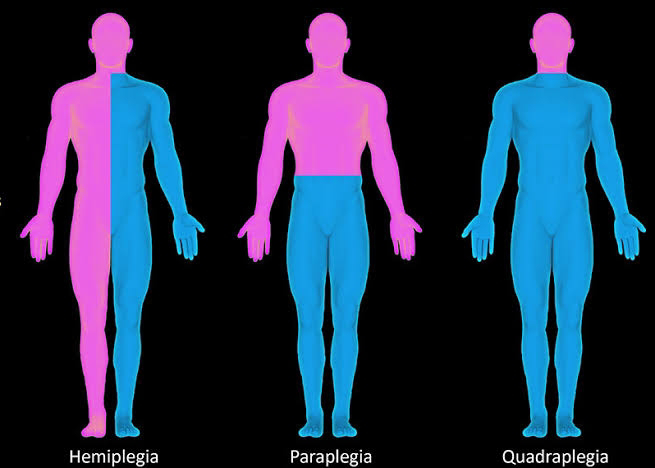
Paraplegia is paralysis of both lower
limbs.
- Paralysis - complete or partial
loss of muscle function leading to loss
of ability to move.
- The loss of muscle function occurs
when there is damage to its nerve supply.
- The motor pathway innervating the muscles consists of Upper motor
neuron (UMN) and lower motor neuron
(LMN).
- The UMN originate in the cerebral cortex and travel down to the brain stem or spinal cord to the level of appropriate spinal nerve root .At this point, the lower motor neurons begin in the anterior horn of spinal cord and goes to innervate muscles and glands throughout the body.
- The nerves of lumbosacral spinal cord
supplies the lower limbs. Damage to
this part leads to paraplegia.
⭐⭐ JUST FOR INFORMATION :- ⭐⭐
Neuromuscular transmission :-
(a) Action potential in the nerve ending
causes depolarisation.
(b) This depolarisation causes influx of
calcium ions in the motor neuron
terminal.
(c) This leads to fusion of vesicles
containing acetylcholine with the
pre synaptic membrane . Emptying
of these vesicles causes release of
neurotransmitter acetylcholine in the
synapse.
(d) Acetylcholine binds to the receptors
present on the post synaptic membrane.
(e) This binding leads to generation of
end plate potential. This end plate
potential when reaches threshold,
leads to generation of Action potential by influx of sodium.
(f) This action potential leads to muscle
contraction by a process called
excitation contraction coupling .
2) CAUSE OF PARAPLEGIA :-
It mainly occurs due to damage to spinal cord.
But , sometimes it may also be caused
due to damage to brain or peripheral
nerves or muscle involvement.
(A) Spinal cord related causes :-
(I) Acute paraplegia :-
# Trauma to the spinal cord - leads
to damage to nerves supplying
lower limb.
# Spinal cord infarction due to
- Vasculitis (Inflammation leads to
damage to the vessel supplying
spinal cord, thus impairing the
blood supply.)
- Anterior spinal artery thrombosis
# Transverse Myelitis (It is sensory,
motor or autonomic dysfunction
due to Inflammation of spinal cord
i.e. Myelitis at a level of cord)
- Inflammation may occur due to various causes like:
Autoimmune diseases.
Sarcoidosis.
Vasculitis.
Certain drugs like Cisplatin.
Post vaccine disease.
Idiopathic etc.
# Neuromyelitis optica
- It is an autoimmune inflammatory disease which
causes damage to the myelin
sheath of neurons. This affects
the neuronal conduction.
# Multiple sclerosis
- It is an autoimmune inflammatory disease which
causes damage to the myelin
sheath of neurons. This affects
the neuronal conduction.
(II) Chronic or Subacute paraplegia:-
Lesion can be present in
following spaces:
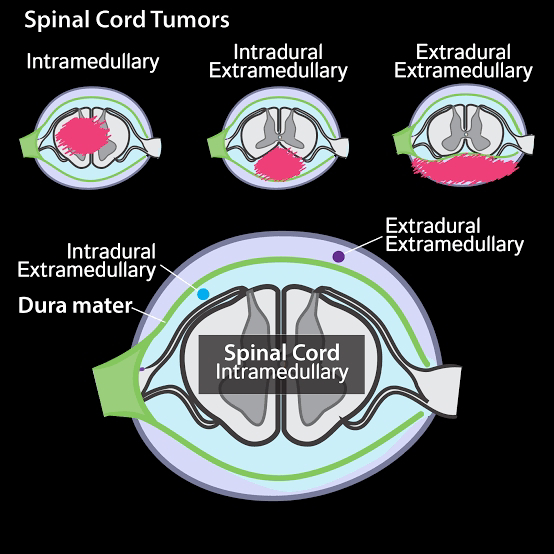
# Extradural cause :- (Due to cord
compression outside the dura
mater. Pressure on the spinal
cord can cause direct damage to
neurons & also damages the
vessels supplying the neurons)
- Spinal metastasis of some
tumors.
- TB spine (Caseating &
granulomatous lesion affecting
vertebrae)
- Primary bone tumor.
- Intervertebral disc proalpse.
- Extra Dural tumors.
# Intra dural extramedullary cause:
- Intraspinal tumors like
meningioma which arises from
meninges.
It causes compression of spinal cord.
# Intra medullary cause:
- Tumors of spinal cord like
Astrocytoma, Ependymoma,
Syringomyelia.
# Miscellaneous causes:
- Subacute combined degeneration (It is a CNS disorder caused due to Vitamin
B12 deficiency. Vitamin B12 is
important for synthesis of
myelin sheath. Thus, impaired
formation of myelin sheath
leads to slowing down or
stoppage of impulses)
- Neurolathyrism (It occurs due
to consumption of legumes
which contain toxin called
ODAP. This toxin causes
damage to motor neuron.)
- Arsenic poisoning (Arsenic is
neurotoxic)
- Fluorosis (It causes damage to
cytoskeleton of neurons)
- Radiation (It causes neuronal
damage)
(B) Cranial causes :-
(I) Sagittal sinus thrombosis -
Superior sagittal sinus drains blood
from lateral and medial surfaces of cerebral hemispheres, including the motor areas for both lower limbs. Hence thrombosis in it causes inability to drain blood leading to compression and damage to these areas resulting in Paraplegia.
(II) Parasagittal Meningioma :-
Leads to pressure over the motor areas for lower limbs .
(C) Lower motor neuron causes :-
(I) Guillian barre syndrome :-
It is autoimmune disorder which
usually occurs after viral infection.
The antibodies destroy myelin
sheath.
(II) Myopathy - muscles are affected
due to fatigue, electrolyte imbalance,
dehydration, immune disorders, etc.
3) CLINICAL FEATURES OF PARAPLEGIA:-
(a) In paraplegia due to acute causes ,
first there is flaccidity of muscles of
lower limb and areflexia.
( Flaccidity - decrease or lack of muscle movement due to nerve damage where the affected body part becomes floppy or without muscle tone and with diminished reflexes.
Areflexia - absence of deep tendon reflexes. Tendons are the tissue that connect muscles to bones. When you tap on a tendon, it causes the muscle to contract and move involuntarily.)
# Flaccidity and areflexia occur initially below the level of the lesion due to interruption of the signals sent via the upper motor neurons to the lower motor neurons or related interneurons due to damage to spinal cord. This period is known as
spinal shock.
(b) After few days or weeks , spinal
shock starts to resolve with development of spasticity and
exaggerated tendon reflexes.
# Reason for this -
- There is recovery of motor neuron
excitability.
- There is increased denervation hypersensitivity .
Denervation ( i.e loss of nerve supply) leads to an initial decrease in number of neuronal membrane receptors, followed by an gradual increase in number, with enhanced sensitivity to neurotransmitters.
This leads to denervation hypersensitivity.
- Gradual changes in muscle properties also occur following Spinal cord damage, such as fibrosis, atrophy of muscle fibers, decrease in the elastic properties, decrease in the number of sarcomeres, accumulation of connective tissue, and alteration of contractile properties.
All these anatomical changes lead to increased muscle tone which likely contribute to the increased passive tension on stretching the muscle as compared to the tension produced on stretching normal muscle.
- This increased passive tension on stretching of affected muscle fibres leads to hyperexcitability of tonic component of stretch reflex which further results in increased muscle tone .
- α-motoneurons after an UMN lesion are known to release growth factors locally . These promote local sprouting from neighbouring interneurons leading to formation of new abnormal synapses which can also contribute to spasticity.
- Tendon hyper-reflexia is identified as an exaggerated muscle response to an externally applied tap of deep tendons. Reduced inhibition of nerve fibres due to spinal cord damage is thought to play an important role in this hyper-reflexia.
- local sprouting of neurons in response to injury can also lead to formation of new abnormal synapses . This can also lead to abnormal reflex pathway production.
(c) In chronic cases of paraplegia - spastic paralysis is seen because there is no sudden interruption of the signals sent via the upper motor neurons to the lower motor neurons.
Eg. Tumor compressing spinal cord - there is gradual damage to neurons. The processes of neuronal damage and production of denervation hypersensitivity are occur simultaneously i.e at one place there may be damage occuring while at the same time, production of hypersensitivity and changes in muscle properties may be occurring at other place.
(d) There are two types of spastic paraplegia :-
(I) Paraplegia in extension :-
increase in the extensor muscle tone leading to extension of limb.
- It occurs in initial stages of damage or when only partial damage to spinal cord has occurred.
- There may be damage to pyramidal i.e corticospinal tract.
- Extrapyramidal tracts are not damaged. Vestibulospinal tract innervates antigravity muscles i.e extensors of leg via LMN.
Thus they cause contraction of the extensors leading to extension of legs.
(II) Paraplegia in flexion :-
- flexion of limbs occur
- it occurs in the later stages of damage when the damage progresses throughout the spinal cord.
- Both pyramidal and extrapyramidal tracts may be affected.
- It may be associated with mass reflexes (exaggerated flexor spasms).
- After an acute, complete Spinal cord damage, flexor reflex excitability develops.
-Dorsal reticulospinal tract which is a part of extrapyramidal tracts has inhibitory control over the stretch reflex through the activation of inhibitory circuits in the spinal cord. It reduce the excitability of the stretch reflex. Thus, damage to these extrapyramidal tracts leads reduced inhibition of flexion reflex leading to hyperreflexia.
4) INVESTIGATIONS OF PARAPLEGIA:-
(I) X-Ray, CT, MRI - to see lesions, tumor.
(II) CSF study - to detect infection.
5) COMPLICATIONS OF PARAPLEGIA:-
(I) Renal infection -Most patients with spinal cord injury have urinary stasis due to neurogenic bladder, which promotes bacterial colonization.
(II) Renal calculi - infection of the urine by urea-splitting organisms, principally Proteus lead to formation of struvite stones.
(III) Fecal impaction - injury below T-12 results in damage to defecation reflex. When the bowel fills with stool the sacral nerves try to send a signal to the spinal cord to defecate but the injury disrupts the signal.
(IV) Pressure sore - Sitting or lying in the same position will begin to cut off the flow of blood to that area, blocking oxygen and vital nutrients from maintaining healthy tissue. When the tissue becomes starved to too long a period of time it begin to die and an pressure sore starts to form.
(V) Contracture of limb due to immobilisation.
6) TREATMENT OF PARAPLEGIA:-
(I) Treat the cause.
(II) Bowel care :
# Laxatives.
# If faeces are hard -manual evacuation.
(III) Bladder care :
# Regular urinary catheterization.
# Sometimes, urinary diversion
technique is needed.
# Treatment of urinary tract infection
& calculi, regular fluid intake.
(IV) Skin care :
# Pressure sores should be prevented by changing the positions
regularly, air or water cushion.
# If pressure sore occurs - treatment
by antibiotics, skin grafting.
(V) Paralysis care :
# Spastic paralysis may lead to
contracture.
# Regular passive movements
should be done.
# Drugs - Baclofen (skeletal muscle
relaxant)
# In severe case - Intrathecal
Baclofen in spinal canal.
(VI) Rehabilitation.
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐





Explanation 10/10✨✨ Well done
ReplyDeleteDr.Nikita
Very well explained Dr.Nikita.👍👍👍 keep it up.
ReplyDeleteThank you so much 😊😊
Delete👌👌👍👍
ReplyDeleteThank you so much 😊😊
Deleteबहुत अच्छा लिखाण
ReplyDeleteThank you so much 😊😊
DeleteVery nice beta
ReplyDeleteThank you so much 😊😊
DeleteYou write so fluently ma'am 👌👌👌 on all the topics
ReplyDeleteThank you so much 😊😊
DeleteNice
ReplyDeleteThank you so much 😊😊
DeleteVery much Impressive madame
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteالكتابة بلغة سهلة هي قوتك. استمر في ذلك يا دكتور نيكيتا
ReplyDeleteThank you so much 😊😊
DeleteWell Explained
ReplyDeleteVery well presentation
ReplyDeleteKeep it up
ReplyDeleteThank you so much 😊😊
Deleteअतिसुन्दर लेखन शैली है आपकी👍😊
ReplyDeleteCongratulations
ReplyDeleteThank you so much 😊😊
DeleteClassy
ReplyDeleteSuperb✨✨
ReplyDeleteThank you so much 😊😊
DeleteVery well written!
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteखुप छान👌
ReplyDeleteThank you so much 😊😊
Deleteनाइस
ReplyDeleteThank you so much 😊😊
Deleteबढ़िया निकीता पाटिलजी👌👌
ReplyDeleteThank you so much 😊😊
DeleteBeta nice work👌
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDelete😊😊 👌
ReplyDeleteThank you so much 😊😊
DeleteJust read it dear👌 Happy to see your variety from Cardiology to neurology.
ReplyDeleteKeep it up.
With love from Berlin❤️
Thank you so much for your appreciation and support sir 😊😊
Delete