⭐⭐ CHRONIC RENAL FAILURE⭐⭐
⭐⭐ CHRONIC RENAL FAILURE ⭐⭐
( CHRONIC KIDNEY DISEASE )
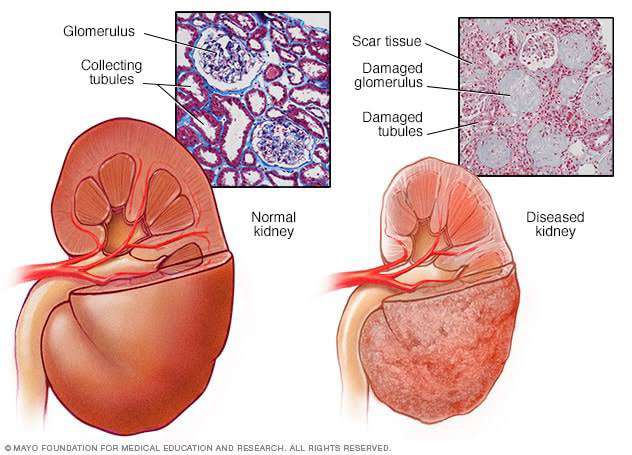
CRF is chronic and irreversible deterioration of kidney function for atleast
> 3 months with GFR < 15 ml/ min/ 1.73 sq metres of body surface area.
2) CAUSES OF CRF :-
(I) Glomerulonephritis :-
It is the inflammation of glomeruli.
GN occurs due to various causes like - post streptococcal GN,
- As a part of autoimmune diseases like SLE, Wegener's granulomatosis ,etc
- Due to primary glomerular disease like cresentic GN, membranous GN, Diffuse proliferative GN.
GN occurs due to deposition of circulating immune complexes or deposition of antibodies due to above causes which may act against antigens in glomerular basement membrane ( molecular mimicry)
(II) Chronic pyelonephritis ( reflux nephropathy ) :-
- Normally during micturition, urine doesn't go back into the ureters from bladder because ureters open in the bladder obliquely and thus the openings get closed during bladder contraction.
- But, if there is defect in the opening of ureters into bladder, reflux of urine may occur.
- Reflux may be due to congenital abnormality of ureteric opening or due to some obstruction at the bladder neck resulting in accumulation of urine in bladder and it's reflux into ureter.
- Due to the reflux, bacteria from the bladder reach the kidney and cause infection and Inflammation leading to scarring of the kidney.
(III) Polycystic kidney disease (PCKD) :-
- It is a autosomal dominant disease.
In about 90 percent of these cases, an affected person inherits the mutation from one affected parent .
- Just for information :-
In PCKD, there is mutation in genes PKD1 and PKD2 .
PKD1 and PKD2 normally code for polycystin i.e PC1 and PC2.
PC1 acts as receptor on the plasma membrane and PC2 on the endoplasmic reticulum (ER) of kidney cells .
Polycystin-1 is activated in response to an extracellular stimulus and interacts with polycystin-2.
The signaling results in activation of calcium channels and increases in cytosolic calcium. Increase in cytosolic calcium initiates signaling cascades that lead to changes in gene transcription. Calcium plays a crucial role in regulating the events of cellular division and apoptosis .
In PCKD, there is mutation in PKD gene resulting in defective polycystin formation which disrupts the calcium signalling.
Dysregulation of calcium signaling due to loss of polycystin function causes the aberrant activation of different pathways associated with abnormal cell proliferation and fluid secretion, thereby leading to the development and expansion of kidney cysts.
(IV) Renal tuberculosis :-
- Renal TB is usually secondary, primary site may be in the lungs.
- The TB bacilli enter the kidney through the blood. They enter glomeruli and cause Granulomatous inflammation in kidney.
(V) Diabetic nephropathy :-
Metabolic and hemodynamic derangements that occur in Diabetes lead to the activation of some signaling pathways and transcription factors, thus triggering the production of cytokines, chemokines, and growth factors, which cause renal damage.
Metabolic factors involve formation of advanced glycation end‐products, activation of protein kinase c and generation of ROS.i.e reactive oxygen species. Higher than normal blood glucose levels and glycation end products cause inflammation. During inflammation, macrophages and lymphocytes can generate reactive oxygen species and Ang II.This ROS damages kidney.
Hemodynamic factors include components of Renin Angiotensin system.
Angiotensin II is increased during diabetic nephropathy. Diabetic nephropathy being an inflammatory condition, macrophages and lymphocytes can generate reactive oxygen species and Ang II .
Ang II causes hypertrophy of various renal cells and has a pressor effect on arteriolar smooth muscle resulting in increased vascular pressure and vasoconstriction.
Rise in Ang II also activates immune cells and causes production of chemokines leading to further renal damage.
These contributing factors cause pathological damage to glomeruli as well as tubulointerstitium
TGF- BETA mediates profibrotic effect to stimuli like hyperglycemia and angiotensin II leading to excess ECM i.e extracellular matrix accumulation and fibrosis in kidney.
Glucose ( metabolic factor) increases BP by impairing the autoregulation of the glomerular microcirculation.
On the other hand, glomerular capillary hypertension ( hemodynamic factor ) enhances GLUT-1 expression leading to increase in intracellular glucose accumulation, thus causing a vicious cycle.
(VI) Tubulointerstitial disease :-
Tubulointerstitial nephritis is inflammation that affects the tubules of the kidneys and the tissues that surround them (interstitial tissue).
- Tubulointerstitial nephritis occurs due to allergic reaction to some drugs like NSAIDS and sulphonamides.
- This disorder may also be caused due to some diseases or toxins that damage the kidneys.
- There is immune mediated infiltration of the kidney interstitium by inflammatory cells. Injury to renal cells leads to expression of new local antigens, inflammatory cell infiltration, and activation of proinflammatory cytokines.
(VII) Obstructive uropathy. ( hydronephrosis) :-
Obstructive uropathy is a condition in which the flow of urine is blocked. This causes the urine to back up into the kidneys and damages the renal parenchyma due to compression and infection.
Causes of obstructive uropathy include :-
- Stones in bladder or ureter
- Benign prostatic hyperplasia
- Prostate cancer
- Bladder cancer
- Scarring of ureter
- Neurogenic bladder
(VIII) Analgesic nephropathy :- It is
damage to the kidney caused by long-term use of analgesics especially acetaminophen, and nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen.
- NSAIDS decrease prostaglandin production. PGs normally increase the blood flow to the kidney by causing vasodilation. Absence of PGs leads to decreased blood flow to the kidney resulting in renal papillary necrosis.
- Paracetamol
In cells of the kidney, cyclooxygenases catalyse the conversion of paracetamol into N-acetyl-p-benzoquinoneimine (NAPQI).
NAPQI depletes glutathione (antioxidant) via non-enzymatic conjugation with glutathione. With depletion of glutathione, cells of the kidney become particularly sensitive to oxidative damage.
(IX) Nephrocalcinosis
Nephrocalcinosis is a disorder in which there is too much calcium deposited in the parenchyma of kidneys. Calcification is the result of deposition of calcium salts within necrotic tissue . It is caused by a number of disorders that cause elevated calcium levels in the blood. Causes include
- Hypercalcaemia
- Hyperparathyroidism
- Vit D therapy
- Hyperphosphaturia
- Sarcoidosis
- chronic Glomerulonephritis
Etc
(X) Hypertensive nephrosclerosis
-It is a disorder that is usually associated with chronic hypertension. There is progressive kidney damage caused by long-standing, poorly controlled high blood pressure .
-Chronic hypertension results in narrowing of preglomerular arteries and arterioles, with a consequent reduction in glomerular blood flow because high blood pressure puts force against the artery walls. Over time, this extra pressure can damage the arteries, making them more vulnerable to the narrowing. Decreased blood to the kidney causes damage.
- Person may develop symptoms of chronic kidney disease such as loss of appetite, nausea, vomiting, itching, and confusion.
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐
3) CLINICAL FEATURES OF CHRONIC RENAL FAILURE :-
(I) Nausea , vomiting and anorexia :- Nausea and vomiting can occur as kidney function decreases. This can be due to the build-up of wastes in your body or a side effect from dialysis or medication. This may lead to a loss of appetite, and weight loss.
(II) Anemia :-
(a) Causes of anemia are as follows:-
- Erythropoietin is produced by kidney. It helps in erythropoesis. In CRF, production of Erythropoietin is decreased leading to decrease in RBC production.
- CRF causes Uremia i.e raised level in the blood of urea and other nitrogenous waste compounds that are normally eliminated by the kidneys. This Uremic toxin causes suppression of the bone marrow cells leading to decreased erythropoesis.
- Hepcidin is a protein produced primarily by the liver and secreted into the circulation. Its levels are increased in patients with chronic kidney disease (CKD) due to diminished renal clearance and an inflammatory state.
Increased hepcidin production in response to inflammation is likely a host defense mechanism to stop iron from invading pathogens. Different cytokines cause increase in hepcidin production by inducing certain signalling pathways.
Hepcidin is a regulator of iron metabolism. It decreases absorption of iron from the intestine by binding to the iron export channel ferroportin located on gut enterocytes and inhibiting it.
Thus decreased iron absorption leads to anemia.
(b) Symptoms of anemia may include:-
fatigue, skin pallor, shortness of breath, dizziness or fast heartbeat.
(III) Renal Osteodystrophy
(a) It includes osteomalacia, hyperparathyroid bone disease, osteoporosis ,osteosclerosis.
(b) Osteomalacia :- Osteomalacia means "soft bones." Osteomalacia is a disease that weakens bones and can cause them to break more easily.
- In CRF, there is decreased production of enzyme 1- alpha hydroxylase
( This enzyme is produced by kidney and it converts 25- OH Cholecalciferol into
1,25 - dihydroxy cholecalciferol i.e active form of vitamin d)
Thus , active form of vitamin D is not formed. This leads to decreased absorption of calcium from intestine. Low levels of calcium affects bone mineralisation leading to osteomalacia.
(c) Low serum calcium and high phosphate levels (due to decreased excretion of phosphate by the damaged kidney ) leads to stimulation of parathyroid gland causing secondary hyperparathyroidism. Hyperparathyroidism leads to loss of calcium from the bone to compensate for the low Calcium level in the blood. This causes further deterioration of the bone.
(d) Osteoporosis and osteosclerosis :-
- On X-ray , sclerotic and porotic patches are seen called rugger jersy spine.
(e) Symptoms may be:
- Bone pain
- Joint pain
- Bone deformation
- Bone fractures
- Poor mobility
Symptoms may not appear early in the course of disease .
Early indicators of renal osteodystrophy include high phosphorus ( due to decreased excretion of phosphate by the damaged kidney) , and/or high PTH levels, red eyes (the accumulation of minerals may settle in the eyes.), itching and sores resulting from calcium-phosphorus deposits.
(IV) Neuropathy :-
(a) Peripheral neuropathy :- It may be sensory, motor or autonomic.
- Symptoms may include :- pain , loss of sensation and ulcer formation, weakness , reduced or absent tendon reflexes, atrophy of muscle, etc.
- Causes of neuropathy include:-
# Uremic toxin ( urea, creatinine, uric acid, guanidine, etc ) can have neurotoxic effect.
# Hyperkalemia occurs in CRF due to decreased excretion of potassium. It also affects the nerves.
In hyperkalemia, as potassium levels increase in the extracellular space, the magnitude of the concentration gradient for potassium across the plasma membrane diminishes, hence less potassium comes out of the cell during repolarization thus decreasing the resting membrane potential (that is, –90 mV to –80 mV )due to increased retention of more positive charge inside the cell and the membrane becomes partially depolarized. Initially, this increases membrane excitability. However, with prolonged depolarization, the cell membrane will become more refractory and less likely to fully depolarize thus decreasing impulse production and neurotransmission.
(b) Apart from Neuropathy, encephalopathy may also occur.
- Symptoms may include :-
Weakness, irritability, altered concentration, focal or generalized motor disturbances, seizures, tremor, delirium, hallucinations, coma.
- Causes include :-
# It may be caused due to accumulation of Uremic toxin like guanidino compounds(GC)
GCs cause activation of excitatory NMDA receptors, and they also cause inhibition of inhibitory GABA receptors thus leading to depolarizing effects.
# PTH can also cause brain damage by increasing brain Calcium. High Ca2+ levels (hypercalcemia) can block sodium movement through voltage-gated sodium channels, causing reduced depolarization and impaired action potential generation. .
# Loss of water soluble vitamins due to dialysis may also cause encephalopathy.
( Wernickes encephalopathy)
# Hypertensive encephalopathy
hypertensive encephalopathy are due to increased cerebral perfusion from the loss of blood-brain barrier integrity, which results in exudation of fluid into the brain.
In normotensive individuals, an increase in blood pressure induces cerebral arteriolar vasoconstriction, thereby preserving a constant cerebral blood flow and an intact blood-brain barrier. This is known as autoregulation of BP.
In chronically hypertensive individuals, this autoregulatory range is gradually shifted to higher pressures as an adaptation to the chronic elevation of systemic blood pressure. But during a hypertensive emergency, in which there is acute rise in blood pressure, the pressure exceeds the autoregulatory range, resulting in hydrostatic leakage across the capillaries within the central nervous system - edema and microhemorrhages.
# Graft rejection immune response can also cause damage to brain due to Inflammation.
# Sepsis in patients of dialysis can cause brain damage due to inflammatory mediators.
# Dialysis can cause rapid changes in osmotic gradient between brain and blood leading to cerebral edema.
# Fluid and electrolyte disturbances can cause osmotic changes and thus brain damage
# Drug toxicity
# Anemia lead to decrease in oxygen supply to the brain.
(c) Stroke can also occur - blood supply to the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.
- Symptoms include :-
# Sudden onset of weakness or numbness on one side of the body.
# Sudden speech difficulty or confusion.
# Sudden difficulty seeing in one or both eyes.
# Sudden onset of dizziness, trouble walking or loss of balance.
# Sudden, severe headache with no known cause.
- Risk factors are
# Hypertension - It causes direct damage to arterial wall due to pressure and thus leads to clot formation.
CRF leads to Hypertension because of sodium dysregulation, increased sympathetic nervous system and alterations in renin angiotensin aldosterone system activity.
# Hypercholesterolemia causing vascular injury due to plaque formation.
HDL cholesterol ( good cholesterol) slows the formation of atherosclerotic plaques in arterial intimal walls.
In chronic kidney dysfunction, HDL cholesterol levels decrease due to the loss of molecules for maturation of HDL cholesterol.
HDL cholesterol deficiency causes increase in foamy cells (lipid-laden macrophages that contain cholesterol. These can form a plaque that can lead to atherosclerosis )
HDL cholesterol dysfunction also causes proinflammatory effects and has a role in progression of CKD. Triglyceride levels can also increase in CRF , due to both increased production and decreased catabolism.
# Bleeding diathesis can also lead to stroke - In CRF , there is decreased platelet activation and impaired adhesion to vascular subendothelial cells.
This is because under normal conditions, ADP and serotonin are secreted to attract more platelets. In renal failure patients, their platelet granules have decreased levels of ADP and serotonin.
# anemia - lead to decrease in oxygen supply to the brain.
Cause of anemia in CRF is explained above.
# bone mineral disorder - Hyperparathyroidism in CRF leads to the increase in calcium in blood which triggers a rise in blood pressure.
Increased influx of calcium into the vascular smooth muscle cells leads to an increased muscular tone and therefore increased vascular resistance and rise in blood pressure.
# Dialysis - In this case, Encephalopathy is likely to be caused by multiple metabolic derangements due to dialysis.
# Metabolic disorders, particularly related to calcium and phosphate which occurs in CRF can also cause stroke. Phosphate and calcium can narrow your blood vessels and increase your risk of stroke.
# Hyperhomocysteinaemia :-
Elevated homocysteine levels are a risk factor for formation of blood clots in the arteries and veins. Homocysteine also has a direct neurotoxic effect .
Hyperhomocysteinemia occurs in CKD patients because of impaired renal metabolism and reduced renal excretion.
# Inflammation and oxidative stress in CRF exacerbate endothelial dysfunction and accelerate atherosclerosis.
(V) Myopathy :-
Conditions like sepsis, ischemia , hypertension and toxins induce acute mitochondrial damage. Uremic toxins CKD also induce mitochondrial damage. Mitochondrial damage leads to decreased exercise capacity, skeletal muscle weakness, and muscle atrophy due to impaired mitochondrial respiratory function and decreased energy production in skeletal muscle.
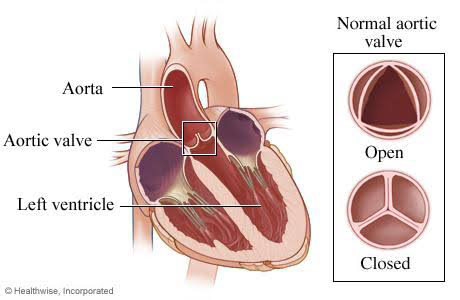
(VI) Pericarditis :-
Uremic pericarditis is thought to result from inflammation of the pericardium by metabolic toxins that accumulate in the body due to kidney failure.
Symptoms include Chest pain , dyspnea
(VII) Pruritus :- itching
Immune system dysfunction, electrolyte imbalance and elevated proinflammatory cytokines are involved in the pathogenesis of pruritus in CKD.
(VIII) Amenorrhea :-
In patients with CKD, the lack of appro- priate cyclic release of gonadotropin releasing hormone (GnRH) by the hypo- thalamus occurs, what leads to a loss of normal pulsatile release of luteinizing hormone (LH) by the pituitary gland. This leads to anovulation and amenorrhea.The cause of impaired cyclic release of GnRH may be hyperprolactinemia, reduced clearance of GnRH and LH ,etc.
(IX) Electrolyte abnormalities :-
Hyperphosphatemia - due to decreased excretion of phosphate by the damaged kidney.
Hypocalcemia :- Hypocalcemia in chronic renal failure is due to two primary causes - increased serum phosphorus ( it forms complex with calcium and gets deposited in bone and other tissues ) and decreased renal production of 1,25 (OH)2 vitamin D.
Hyperkalemia :-
Hyperkalemia occurs in CRF due to decreased excretion of potassium.
(X) Hypertension :-
- Causes of Hypertension include:-
(I) The inability to excrete sodium and water via the damaged kidneys contributes to increased extracellular volume, increased cardiac output, and increased BP .
(II) Higher concentration of sodium in dialysate is being used to reduce hemodynamic and osmotic disequilibrium.
Exposure to large dialysate to plasma sodium gradients that favor diffusion of sodium into the patient may cause hypertension .
(III) Elevated plasma Renin activity (RAAS) also contributes to hypertension. Angiotensin II (Ang II) and aldosterone, which are primary mediators of RAAS, both contribute to endothelial cell dysfunction .
(IV) CKD patients have higher sympathetic nervous system (SNS) activity , mean arterial BP, and vascular resistance .
This is because of renal ischemia, signaling from diseased kidneys that results in elevated sympathetic activity and renal afferent nerve activation and HTN . Changes in levels of Nitric oxide, angiotensin II, and superoxide may further modify the SNS response.
(V) Endothelial cell-derived nitric oxide (NO) causes vasodilation and endothelin-1 (ET-1) cause vasoconstriction, upon binding to vascular smooth muscle cell receptors.
Endothelial cell dysfunction (ECD) involves disrupted balance of these mediators, with increased vasoconstriction .
Furthermore, NO release can be reduced by the actions of inhibitor of NO synthase.Reactive oxygen species (ROS) can also interfere with NO synthesis and availability.
(VI) Hyperparathyroidism that accompanies CKD may contribute to HTN due to increased platelet cytosolic calcium.
(XI) Metabolic acidosis :-
Metabolic acidosis is commonly found in patients with chronic kidney disease (CKD), and its causes are:
impaired ammonia excretion,
reduced tubular bicarbonate reabsorption and insufficient renal bicarbonate production ( more ammonia and less bicarbonate ) in relation to the amount of acids synthesised by the body and ingested with food.
Diagnosis is made by :-
# measurement of serum electrolytes
# Arterial blood gas analysis (ABGA), which shows pH and PaCO2 to be low; HCO3- also is low.
Symptoms are as follows :-
rapid and shallow breathing -Faster breathing helps expel more carbon dioxide, which is an acidic compound in your blood.
confusion - brain hypoxia and acidosis play an important role in the development of cerebral edema and brain damage.
fatigue
headache
sleepiness
lack of appetite
jaundice
increased heart rate
(XII) Infection :-
It occurs due to decreased immunity.Acute renal failure has a severe impact on the immune system due to Uremic toxins and immunosuppressive drugs .
(XIII) Uremic encephalopathy :- explained in neuropathy above.
(XIV) Complications of dialysis :-
(a) Hypotension - Due to rapid loss of fluid from blood during dialysis, the blood volume decreases leading to hypotension.
(b) Muscle cramping - Due to hypovolemia, there is decreased perfusion of the muscles which causes imbalance of potassium & calcium between ECF & ICF leading to muscle cramps.
(c) Anaphylactoid reaction to dialysate.
(d) Infection due to contaminated dialysate.
(e) Air embolism.
(f) Cardiac problems.
(g) Dialysis disequilibrium syndrome - neurological symptoms caused by rapid removal of urea during hemodialysis. It develops primarily from an osmotic gradient that develops between the brain and the plasma as a result of rapid hemodialysis.
This leads to cerebral edema.
Symptoms include :- Nausea, vomiting, headache, hypertension, seizures, coma.
(h) Dementia - Due to Aluminium in dialysate.
(i) Wernicke's Encephalopathy - Due to Vitamin B1 loss from blood into dialysate.
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐
4) INVESTIGATIONS OF CHRONIC RENAL FAILURE:-
(I) Urine microscopy :-
Presence of
- Red cells = Glomerulonephritis
- WBCs = infection, tubular necrosis.
- Eosinophils = Allergic nephritis
(II) Hematocrit = anemia
(III) Biochemical abnormalities =
Increased urea, creatinine, phosphate, potassium.
Decreased calcium
(IV) X ray abdomen = tells about kidney size, obstructive uropathy .
(V) USG = shrunken kidney
( Normal kidney is seen in cases of amyloidosis, Polycystic kidney disease, diabetic glomerulosclerosis )
(VI) CT scan
(VII) Percutaneous renal biopsy
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐
5) TREATMENT OF CHRONIC RENAL FAILURE:-
(I) CONSERVATIVE MANAGEMENT :-
(a) Control of BP - below 140/90 mm of Hg . Give ACE inhibitors.
(b) Diet management :-
- Salt restriction
- Protein intake upto 40gm / day, not more than that.
- Don't eat potassium rich food.
If there is severe hyperkalemia, potassium exchange resins are used.
(c) Treatment of hypocalcemia :-
Calcitriol + Calcium supplementation.
Moniter serum calcium levels.
(d) Treatment of hyperphosphatemia:-
Phosphate binders ( They prevent PO4 absorption in gut) = Calcium carbonate, calcium acetate , sevalamer carbonate, lanthanum carbonate.
(e) Acidosis = Calcium carbonate + Sodium bicarbonate.
(f) Anemia = Erythropoietin + iron supplement ( if required, add folate, vit B12 ) Monitor BP.
(g) Treatment of Hyperparathyroidism:
- Calcimimetic = Cinacalcet
It mimics the action of calcium by binding to Calcium sensing receptors ( CaSR) on parathyroid gland.
Gland senses that there is lot of calcium in the blood. Therefore PTH secretion decreases.
- Calcium carbonate , acetate = to bind CaSR.
(II) DIALYSIS :- Done when conservative treatment fails.
Indications are as follows :-
- Severe Acidosis
- Pulmonary edema
- Uremic pericarditis
- Uremic encephalopathy
- Severe hyperkalemia
(III) RENAL TRANSPLANTATION
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐


👌👌nice
ReplyDeleteThank you so much 😊😊
Deleteनेहमी प्रमाणे अप्रतिम लिखाण आहे. एवढ्या लहान वयात इतकी प्रतिभावान बुद्धिमत्ता हे amazing आहे. तुझ्या लिखाणात खंड पडू देऊ नकोस. सरळ व साधी भाषा हे तुझ्या लिखाणाचे वैशिष्ठ्य आहे. मेडिकल सायन्स मधील प्रत्येक विषय तू अगदी सहजरित्या हाताळत आहेस. बेटा तुला माझ्याकडून खूप खूप शुभेच्छा.
ReplyDeleteThank you so much madam for your support and appreciation🤗🤗 It really means a lot
DeleteEtiopathogenesis part was the best👌👌
ReplyDeleteThank you so much 😊😊
DeleteVery informative, nice. Keep it up. Dr. Nikita🙂
ReplyDeleteThank you so much 😊😊
DeleteNice to read your articke
ReplyDeleteThank you so much 😊😊
Delete👌👌
ReplyDeleteThank you so much 😊😊
DeleteVery very informative. Was waiting to read all the busy schedule. Keep it up dear
ReplyDeleteThank you so much for your appreciation 😊😊 please keep supporting
DeleteGood job
ReplyDeleteThank you so much 😊😊
DeleteVery nice
DeleteThank you so much 😊😊
Deleteबेटी लेखन खुप च कौतुकास्पद आहे👍
ReplyDeleteThank you so much 😊😊
DeleteGood job drnikita
ReplyDeleteThank you so much 😊😊
DeleteAge youth but content mature👌👌 Goodwork
ReplyDelete👍
ReplyDeleteThank you so much 😊😊
DeleteNice work
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteबेटा किती बुद्धिमान आहेस👌👌 प्रस्तुत करण्याची कला अप्रतिम आहे
ReplyDeleteThank you so much 😊😊
DeleteKhub bhalo
ReplyDeleteThank you so much 😊😊
DeleteGood
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteGood writing
ReplyDeleteअप्रतिम आहे पोरी👌 वाचायला वेळ मिळत नव्हता. आज वाचला. खुप चांगल explain केलंस
ReplyDeleteThank you so much madam for reading my post regularly and encouraging me🙏😊😊
DeleteLoved the explanation👌
ReplyDeleteThank you so much 😊😊
Delete👍👍 well done beta
ReplyDeleteThank you so much 😊😊
DeleteNice work doing
ReplyDeleteThank you so much 😊😊
DeleteGood,
ReplyDeleteThank you so much 😊😊
DeleteSuperb!
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteNice work beta
ReplyDeleteThank you so much 😊😊
Delete👌👌👌👌
ReplyDelete😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteGirl. You are doing a fabulous job. Keep it going sweetie. Never let anyone fall you down. Never get upset. I Repeat NEVER. People are always there to pull your legs, but an Elephant don't lose his majesty when dogs bark. So always stay motivated. Work hard. Go! Love from Berlin.
ReplyDeleteThank you so much sir for your support and motivation 😊😊 No doubt it acts as an energy booster... I needed this type of motivation which I got very few times upto now 🙏🙏
DeleteVery nice
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDelete👌👌👌
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDelete