⭐⭐CONSTIPATION⭐⭐
⭐⭐ CONSTIPATION ⭐⭐
1) DEFINITION OF CONSTIPATION :-
Any 2 of the following criteria should be
present for >12 weeks :-
(a) Less than 3 defecations in a week
(b) Straining for > 25% defecations
(c) Hard stools for > 25% defecations
(d) Sense of incomplete evacuation for
> 25% defecations
(e) Sense of anorectal blockade for
> 25% defecations
(f) Digital evacuation of stools (by
fingers) for > 25 % defecations.
⭐ There are no loose stools in constipation⭐
⭐⭐⭐⭐⭐⭐⭐
2) CAUSES OF CONSTIPATION :-
(a) Acute causes :- (I) Dehydration :-
Water in the stool makes it softer
and helps it to pass more smoothly.
When there is dehydration, stools
become dry and hard .
Hence, dehydration is a common
cause of constipation.
(II) Acute Intestinal obstruction :-
Obstruction in the bowel halts the
process of formation and elimination
of stools.
Eg - Obstruction due to adhesions,
tumors, hernia ,fecal impaction
gall stones,etc.
(III) Acute appendicitis :-
Inflammation causes damage to
the tissues and affects bowel
movements.
(b) Chronic causes :-
⭐ Functional causes :- (voluntary
withholding of stools)
(I) Rectal stasis of stools due to -
# Faulty habits - not emptying the
bowel regularly
# Unconsciousness - there is
constipation due to obstructed defecation, weak abdominal
muscles, impaired rectal
sensation and delayed colonic
transit time.
# Anal fissure - due to pain &
spasm of sphincter.
(II) Colonic stasis -
# Inadequate food intake
# Inadequate fibre intake - Fibre
helps to increase the stool weight
by causing water retention in the
stools & thus decreases colonic
transit time & easier evacuation of
stools.
# Endocrine disease
# Irritable bowel syndrome -
- Tension, worries & anxiety may
precipitate this altered bowel
movements.
- In IBS, there may be changes in
how the intestines move &
contract or changes in how the gut
senses pain. There may be
changes in the composition of
bacteria that are normally found
in the gut.
- This may lead to changes in
bowel function & constipation.
⭐ Organic causes -
(I) Endocrine causes -
# Diabetes -
- Hyperglycemia impairs
functioning of enteric neuronal
system and causes autonomic
neuropathy
- Loss of functional ICC cells.
These are pacemaker cells in git
which control neuronal input
from nerves to smooth muscle
cells. Thus , they help to control
intestinal contractions.
- Diabetes causes smooth muscle
myopathy.
# Myxoedema -
- In hypothyroidism , intestinal wall
( muscle layer) is thickened,
thereby increasing the muscle
tone and leading to reduced
intestinal motility
# Hypercalcaemia -
- Calcium deposition in kidney
leads to damage to kidney
leading to decreased sensitivity
of kidney towards ADH ( water
retaining hormone) . This results
in polyuria and dehydration
leading to constipation
- Calcium ion inhibits sodium
reabsorption in PCT and
ascending limb of henle loop
thus leading to increased sodium
excretion . Natreuresis causes
polyuria and thus dehydration.
# Hyperparathyroidism -
- It results in constipation because
of reduction in neuromuscular
excitability by high calcium levels.
High calcium levels can block
sodium movement through voltage
gated Sodium channels leading to
reduced depolarisation & Impaired
action potential generation.
(II) Muscular diseases -
# Amyloidosis -
- Amyloid deposits in GIT can
interfere with function & motility
of the gut.
- It can also affect sensory, motor
or autonomic nerves leading to
their degeneration.
This all leads to decreased bowel
movements.
# Systemic sclerosis -
- It is an autoimmune disorder
leading to neuropathy & myopathy.
This results in dysmotility of gut &
constipation.
(III) Neurological diseases -
# Parkinson's disease -
- Due to changes in dorsal vagal
nucleus function.
- Due to loss of dopaminergic
neurons. (Dopamine helps in
controlling muscle movement)
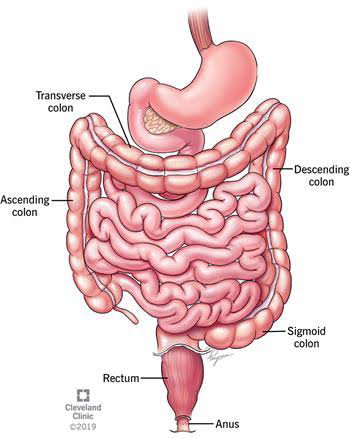
# Hirschsprung disease -
- A part of large intestine lacks
normal nerve cells leading to
impaired motility of intestine.
# Cerebrovascular disease -
- Damaged nerves disrupt the
ability of gut to store & get rid of
waste.
(IV) Structural disease -
# Anal fissure -
- Constipation occurs due to pain
& spasm of spinchter.
# Hemorrhoids (Piles) -
- The swollen blood vessels &
tissue can bleed & cause bowel
movements to become painful.
Thus, leading to constipation.
# Megacolon -
- There is bowel dysfunction as a
result of neurological or muscular
disorders.
# Anal stenosis
(V) Psychological disease -
# Depression -
- Shortage of serotonin in the
neurons of the gut can lead to
constipation. (Serotonin is a
neurotransmitter)
(VI) Others -
# Tumor pressing on the rectum.
(VII) Medications -
# Anticholinergic drugs -
- This medications block the
effect of Acetylcholine, a
chemical that helps the muscles
to move. Thus, less movement in
the gut leads to constipation.
# Antihistaminic drugs -
- This medications block the
action of Acetylcholine.
# Antacids -
- They can cause disturbances in
the gut motility leading to
constipation.
# Calcium Channel Blockers -
- These drugs may cause
relaxation of the muscles in the
gut leading to constipation.
# Calcium -
- (Refer to hypercalcaemia)
⭐⭐⭐⭐⭐⭐
3) MECHANISMS OF CONSTIPATION :-
(a) Primary constipation or functional constipation - occurs due to
defect in colonic function or defect in
anorectal function.
# Normal transit constipation - stool moves through colon at regular
speed.
# Slow transit constipation - stools
take longer time to pass through
the colon . Bowel peristalsis is
decreased.
(b) Secondary constipation - due to
underlying cause
# Diabetes
# Medications
# fissure, piles
# neurological causes like Parkinson's disease ,etc
⭐⭐⭐⭐⭐⭐
4) INVESTIGATIONS OF CONSTIPATION -
A) History taking - Ask about
(I) Bowel habits & Fiber intake.
(II) Water intake. Also examine for
signs of dehydration like skin pinch
test, dryness of tongue.
(III) Medications.
(IV) Psychological causes like
depression.
(V) Ask about structural causes
like piles, fissure, tumor.
(VI) Ask about history of diabetes or
thyroid disease.
(VII) Examine for neurological disease
like Parkinson's disease - Tremors,
Rigidity, Akinesia, Postural Instability.
(VIII) Ask about symptoms like
abdominal pain, bloating, vomiting,
anorexia, etc.
(IX) Ask about history of weight gain
or weight loss, anaemia, blood in stool
suggestive of carcinoma.
(X) Ask about any previous surgery.
(XI) Examine the abdomen by
auscultating for bowel sounds &
palpating for any swelling, pain
tenderness or any masses. Rectal
examination can also be performed.
B) Colonoscopy, Sigmoidoscopy -
To find for
(I) Intestinal obstruction.
(II) Megacolon.
(III) Tumor pressing on rectum.
(IV) Stricture.
(V) Gall stones.
(VI) Fecal impaction.
(VII) Colon carcinoma - Rectal
bleeding, weight loss, anaemia.
C) Stool examination -
- Dry hard stools.
- Decreased amount of stool.
- Tiny rock or pebble like stool.
- Blood in stool indicates carcinoma.
D) CBC -
Inflammatory conditions like
appendicitis, Inflammatory Bowel
diseases.
E) Other-
# Blood glucose - Diabetes.
# Thyroid hormones - Hypothyroidism.
# Serum Calcium - Hypercalcaemia,
Hyperparathyroidism.
# MRI - Cerebrovascular disease.
F) Colon transit time -
It measures how long it takes for
the food to travel through the colon.
Special capsules are taken by mouth
twice a day for 5 days.The capsule
has X-ray markers. Average transit
time is 30 to 40 hrs. Decreased bowel
movement causes increased colon
transit time.
G) Anorectal manometry -
A catheter with balloon on the end is
inserted through the anal opening,
past the anal sphincter. The balloon
is gradually inflated. This causes
nerves & muscles in the rectum &
anus to begin to squeeze. The end of
the tube outside the anus is
connected to a machine that records
the contractions & relaxations of the
rectum & anal sphincter. It measures
how well the rectum & anal
sphincters are working.
⭐⭐⭐⭐⭐⭐
5) TREATMENT OF CONSTIPATION -
A) Treat the underlying cause.
B) Non pharmacological treatment -
(I) Eat fibre rich food - fruits,
vegetables.
(II) Drink plenty of water.
(III) Train the patient to recognise
urge to defecate.
(IV) Advice the patient to defecate in
the morning when the bowel is active
& after 30 mins of meals to take
advantage of gastrocolic reflex.
(V) Maintain diary of no. of
defecations, consistency of stools,
straining, etc.
(VI) Patient should be physically
active - Exercise is necessary because
abdominal wall muscles & diaphragm
play an important role in the process
of defecation.
C) Pharmacological treatment -
(I) Laxatives -
# Ispaghula - It makes the stool
soft by increasing their water
content. It also lubricates the
Intestine which improves the
transit of stools.
# Methyl cellulose - It absorbs water
in the GIT lumen thereby increasing
the bulk of stools.
# Stool softeners (emollient laxative)-
Docusate.
(II) Prokinetic agents -
Cisapride, Mosapride, Prucalopride.
They increase the motility of
intestine.
(III) Linaclotide - It is agonist of
guanylate cyclase- C receptor on the
luminal surface of intestinal
enterocytes. It decreases c- GMP levels
to decrease pain & also accelerates the
gastrointestinal transit.
(IV) Lubiprostone - It stimulates type II
chloride channels in the epithelial cells
causing an efflux of chloride into the
intestinal lumen. The resultant fluid
secretion into the gastrointestinal
lumen provides a bolus effect that
softens the stools & increases the
intestinal transit.
⭐⭐⭐⭐⭐⭐


Very nice article.. Keep enlightening us
ReplyDeleteThank you so much 😊😊
DeleteWas waiting since long time. Thank u ma'am
ReplyDeleteThank you so much for supporting 😊😊
DeleteNicee
ReplyDeleteThank you so much 😊😊
DeleteVery Informative
ReplyDeleteThank you so much 😊😊
DeleteNice & informative article. Keep it up 🙂
ReplyDeleteThank you so much 😊😊
DeleteFruitful and informative article
ReplyDeleteThank you so much 😊😊
Delete👌👌nice
ReplyDeleteThank you so much 😊😊
DeleteGreat content and fairly organised!
ReplyDeleteTry to use colours and fonts while typing, will keep the reader more engaged:)
Thank you so much for your review and support ☺️☺️
DeleteThank you so much 😊😊
ReplyDeleteInformative Stuff.
ReplyDeleteWaiting for more, Nikita.
Thank you so much 😊😊
DeletePresentation perfect dr nikita
ReplyDeleteThank you so much 😊😊
DeleteThank you so much Dr jigisha ☺️☺️
ReplyDeleteGood good good👍👍
ReplyDeleteकाफी वधिया बेटाजी.👌
ReplyDeleteकहां से हो आप?
Thank you so much 😊😊 I am from Maharashtra
DeleteGreat👍👍 big fan
ReplyDeleteThank you so much 😊😊
DeleteBeta u write very beautifully. Keep it up
ReplyDeleteThank you so much 😊😊
DeleteVery much impressed!
ReplyDeleteThank you so much 😊😊
Delete💥💥💥
ReplyDeleteThank you so much 😊😊
DeleteSimply great👌👌👌
ReplyDeleteThank you so much 😊😊
DeleteNever seen such a detailed explanation. Awesome ✨
ReplyDeleteThank you so much 😊😊
Deleteगुड👌
ReplyDeleteThank you so much 😊😊
DeleteBahot acche
ReplyDeleteEnjoyed the article very much👌
ReplyDeleteThank you so much 😊😊
DeleteWriting skills 10/10!
ReplyDeleteDr.Franco Rush,LA
Thank you so much 😊😊
Delete👌👌👌👌 khup chhan
ReplyDeleteখুব ভালো বেটা
ReplyDeleteThank you so much 😊😊
DeleteNice
ReplyDelete👌👌
ReplyDeleteThank you so much 😊😊
DeleteGood one
ReplyDeleteKafi sahi hai!
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteWell done
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteबेटी, खुप सुंदर लिहतेस 👌👌👌 असच लिहत रहा
ReplyDeleteThank you so much 😊😊
DeleteMy bengali friend Sulochna recommended me your blogs. Im amazed by your writing skills. Very well done baccha.
ReplyDeleteLolita Chattopadhyay, Kolkata
Thank you so much madam for reading 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDelete