⭐⭐⭐ ACUTE RENAL FAILURE ⭐⭐⭐
⭐⭐ ACUTE RENAL FAILURE ⭐⭐
( ACUTE KIDNEY INJURY )
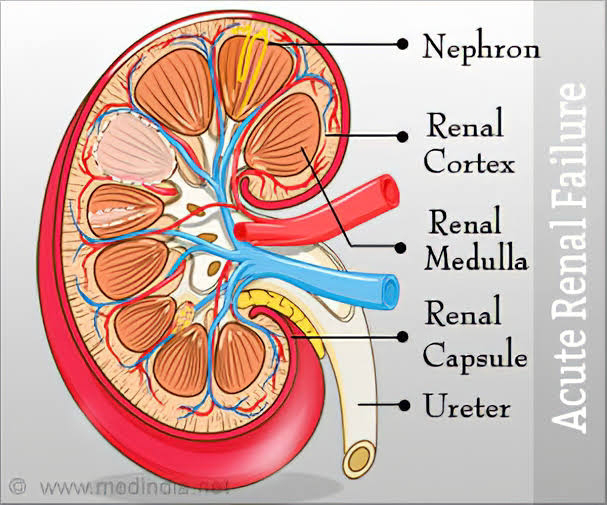
- Kidneys help to filter and remove waste products in the blood.
- It also helps to maintain electrolyte balance.
- kidneys also make hormones that help to control blood pressure (Renin Angiotensin aldosterone system - RAAS),
make red blood cells ( Erythropoetin)
keep your bones strong and healthy ( 1- alpha hydroxylase causes conversion of 25 -OH cholecalciferol to 1,25 - dihydroxy cholecalciferol i.e active form of vitamin D.
2) DEFINITION OF ARF :-
ARF is rapid deterioration of renal function which is enough to cause accumulation of nitrogenous wastes in body.
ARF is also called as AKI i.e Acute kidney injury.
3) RIFLE Criteria :-
(I) R = Risk.
Increase in serum creatinine by ( × 1.5 ) times the normal.
or
Urine output is < 0.5 ml / kg / hr for atleast 6 hours.
(II) I - Injury -
Increase in serum creatinine of (×2) times the normal
OR
Urine output is < 0.5 ml/kg /hr for 12 hours.
(III) F - Failure -
Increase in serum creatinine of (×3)times the normal
OR
serum creatinine > 4 mg/ dl
OR
Urine output < 0.3 ml /kg/ hr for 24 hours
or Anuria for 12 hours.
(IV) L - Loss -
Loss of renal function for > 4 weeks.
(V) E -End stage kidney disease
i.e. Loss of renal function for > 3 months.
# ARF is said to have occurred when
(I) Increase in serum creatinine > 1.5
times in prior 7 days.
OR
(II) Urine output is < 0.5 ml/kg/hr for more than 6 hours.
OR
(III) Increase in serum creatinine > 0.3 mg/dl in two days.
4) ETIOPATHOGENESIS OF ARF :-
(A) PRERENAL CAUSES :-
(I) Hypovolemia :-
- Hypovolemia is a condition in which the liquid portion of the blood (plasma) is too low.
- It occurs in cases like
Haemorrhage
Diarrhoea - loss of water through stools
Vomiting
Burns - loss of plasma
Diuretics - due to increased urine
output
Septic shock - vasodilation due to Infection and inflammation leads to loss of fluid from vessels and results in hypovolemia.
- Kidneys need adequate blood flow to help filter waste products and remove excess fluids. Reduced blood flow to kidneys may injure kidney tissue and lead to renal failure. Kidneys need ATP to maintain cellular functions. ATP drives the active transport of glucose, ions and nutrients. Kidney is one of the most energy-demanding organs in the human body.
Thus, decreased blood flow to kidneys cause deterioration of the kidney functions and damages the tissue due to inadequate supply of substrates like Oxygen , glucose ,etc. This results in kidney failure.
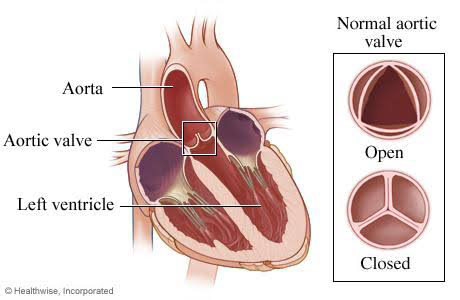
(II) Decreased cardiac output :- due to causes like heart failure.
Decreased cardiac output leads to decreased blood flow to the kidney.
(III) Renal artery obstruction :- caused due to atherosclerosis or injury to renal artery. It leads to decreased blood supply to kidney.
(IV) Drugs :-
(a) ACE inhibitors :-
- Angiotensin II causes vasoconstriction of both afferent and efferent arterioles, but because the efferent arteriole has a smaller diameter, the increase in efferent arteriolar resistance exceeds the increase in afferent arteriolar resistance.
Thus , efferent arteriolar resistance exceeds afferent arteriolar resistance due to Angiotensin II.
- Narrowed efferent arteriole leads to increase in hydrostatic pressure in the glomerular capillaries. This results in increased GFR i.e glomerular filtration rate.
- ACE inhibitors cause both afferent and efferent arteriolar vasodilation.
This vasodilation leads to decreased perfusion to the kidney and can cause renal damage. It also decreases GFR.
(b) NSAIDS (Nonsteroidal anti-inflammatory drugs) :-
- Prostaglandins cause vasodilation of afferent arteriole which leads to increase in renal blood flow.
- NSAIDS decrease prostaglandin production by inhibiting enzyme cyclooxygenase (Cox). Decrease in PGs causes vasoconstriction of afferent arterioles which decreases the blood flow to the kidney causing renal damage.
⭐⭐⭐⭐⭐⭐⭐⭐⭐⭐
(B) RENAL CAUSES OF ARF :-
(main pathology is in the kidney)
(I) Glomerular cause - It includes Glomerulonephritis ( GN) i.e inflammation of glomeruli.
GN occurs due to various causes like - post streptococcal GN,
- As a part of autoimmune diseases like SLE, Wegener's granulomatosis ,etc
- Due to primary glomerular disease like cresentic GN, membranous GN, Diffuse proliferative GN.
GN occurs due to deposition of circulating immune complexes or deposition of antibodies which may act against antigens in glomerular basement membrane.
(II) Tubulointerstitial nephritis :-
-Tubulointerstitial nephritis is inflammation that affects the tubules of the kidneys and the tissues that surround them (interstitial tissue).
. - Tubulointerstitial nephritis occurs due to allergic reaction to some drugs like NSAIDS and sulphonamides.
- This disorder may also be caused due to some diseases or toxins that damage the kidneys.
- There is immune mediated infiltration of the kidney interstitium by inflammatory cells. Injury to renal cells leads to expression of new local antigens, inflammatory cell infiltration, and activation of proinflammatory cytokines.
(III) Vascular causes :-
- These include Vasculitis and renal artery occlusion.
- Vasculitis leads to Inflammation and damage to the vessels which impairs the blood supply of kidney and also leads to damage to the glomrular capillaries. This results in kidney damage.
It may be an autoimmune disease. White blood cells and antibodies (natural defences) that fight off infection are damaging our own body.
- Renal artery occlusion decreases the blood supply to the kidney. It can occur due to atherosclerosis or injury to renal artery.
(IV) Acute tubular necrosis (ATN) :-
- Acute tubular necrosis is a condition that causes damage to the tubules of nephrons of the kidney. It occurs due to lack of oxygen and blood flow to the kidneys thus causing damage.With initial ischemic or cytotoxic injury, a number of tubular cells may undergo apoptosis due to molecular cascades that release TNF-alpha or Fas .
- causes of acute tubular necrosis are conditions like stroke ,heart failure, which reduce oxygen to the kidneys.
Chemicals can also damage the tubules. These include X-ray contrast dye, anesthesia drugs, antibiotics and other toxic chemicals.
Trauma can also lead to ATN
Malaria can also cause ATN due to granular deposits of hemosiderin in tubules and hemodynamic instability.
⭐⭐⭐⭐⭐⭐⭐⭐⭐
(C) POST RENAL CAUSES OF ARF:-
(I) Extrarenal causes (outside the kidney)
- Stones in ureter or bladder :- They can cause obstruction to the flow of urine.
Due to obstruction, there is reflux of urine back into the kidney causing infection and deterioration of function of kidney.
- BPH ( benign prostatic hyperplasia) :- It causes urinary retention in bladder leading to vesicoureteric reflux.
- Urethral stricture :- Causes obstruction to the flow of urine leading to vesicoureteric reflux.
- Tumors in bladder or urethra.
(II) Intrarenal causes ( inside the kidney) :-
- Uric acid crystals:- They can cause damage to kidney by blocking the kidneys from removing wastes, which can cause infection, and scarring the kidneys with their sharp edges.
- Papillary sloughing :- There is necrosis of renal papillae. Renal papillae are the areas where the openings of the collecting ducts enter the kidney and where urine flows into the ureters.
Necrosis of papillae will not allow the urine to flow out of the collecting ducts thus leading to clogging of the urine in the kidney leading to damage to the kidney.
5) CLINICAL FEATURES OF ACUTE RENAL FAILURE :-
( CORRELATE THE CLINICAL FEATURES GIVEN BELOW WITH POINTS IN ETIOPATHOGENESIS )
(A) SYMPTOMS ASSOCIATED WITH PRERENAL CAUSES OF ARF :-
(I) Diarrhoea, vomiting can cause hypovolemia.
If Diarrhoea , vomiting are present, following causes must be suspected and likewise history and examination should be done:-
# gastroenteritis due to Infection - leads to hypovolemia.
# Alcoholism, ( excessive amounts of alcohol can cause an imbalance in electrolytes like sodium, calcium , potassium as well as an acid-base imbalance. These imbalances can eventually lead to acute kidney failure )
# Pregnancy (hyperemesis gravidarum) -
Persistent vomiting can result in volume depletion and lead to renal failure.
# food poisoning - severe dehydration can cause hypovolemia.
# side effects of some medications like certain antibiotics - aminoglycosides, cephalosporins, amphotericin cause direct toxicity to kidney
NSAIDS such as ibuprofen and aspirin ,
chemotherapy drugs ( NSAIDs can reduce renal blood flow and GFR by decreasing prostaglandins thus resulting in ARF. ).
(II) Haemorrhage leading to hypovolemia can be due to
# Injury or trauma ( external bleeding) - blood loss is obvious .
# Internal bleeding may occur in many areas of the body and may cause hypovolemia if bleeding is large enough.
Causes of internal bleeding include :-
- Trauma
- Broken bones
- Pregnancy related - placenta previa, placental abruption leading to Postpartum hemorrhage.
- Bleeding after surgery -sutures, or clips can dislodge and allow a blood vessel to bleed. Surgical procedure on your heart or blood vessels causes changes in blood flow and may increase your risk of acute renal failure after surgery.
- Alcohol - Alcohol abuse can cause liver damage, which may cause bleeding problems due to decreased protein and clotting factor production. Cirrhosis, leads to portal hypertension and formation of varices which tend to bleed.
sympathetic response is stimulated in patients with alcoholic cirrhosis of the liver, as a result of reflex response to the splanchnic vasodilatation and vascular shunting present. Activation of the sympathetic nervous system results in renal vasoconstriction and reduced renal blood flow, leading to progressive renal failure, reduced glomerular filtration, and even ATN.
- Medications - NSAIDS can cause inflammation and bleeding in stomach, duodenum. NSAIDs can reduce renal blood flow and GFR by decreasing prostaglandins thus resulting in ARF.
Symptoms of internal bleeding depend on where the bleeding is coming from :-
# Head - headache,confusion, Paralysis, neck stiffness, vision loss, weakness .
# Intra-abdominal bleeding :-
hemetemesis
blood in stool
Low BP
Shortness of breath
# History of blunt trauma or fracture. Risk factors in this case are patients with diseases like hemophilia, patients taking anticoagulant medications.
(III)- History of diuretic intake in hypertensive patients
(IV) - Septic shock occurs due to Infection.
Symptoms of septic shock :-
Fever or hypothermia
Tachycardia
Tachypnea
Low BP
Oliguria
Confusion, dizziness
Cyanosis
(V) - Decreased cardiac output leads to renal failure . It may present as chest pain, dyspnea, palpitations, sweating, heartburn, vomiting , edema ,etc.
(VI) - Renal artery obstruction may present as
# continued high blood pressure (hypertension) despite taking medications to help lower it.
# decreased kidney function.
# fluid retention.
edema (swelling), especially in your ankles and feet.
# Proteinuria
⭐⭐⭐⭐⭐⭐⭐
(B) SYMPTOMS DUE TO INTRARENAL CAUSE OF ARF:-
(I) Glomerulonephritis :-
- Hematuria, red cell casts in urine ( due to damaged glomeruli.)
- Oliguria ( due to impaired glomerular ultrafiltration)
- Proteinuria ( due to leakage of proteins from damaged Capillaries)
- Uremia ( increased amount of urea in blood)
- Oedema ( due to sodium retention, water retention also occurs causing increased hydrostatic pressure in vessels and leakage of fluid out of the vessels) Sodium retention occurs due to increased reabsorption of sodium in the collecting tubules
- Hypertension ( due to fluid overload )
(II) Tubulointerstitial nephritis due to allergic reaction to drugs :-
- Fever
- Rashes
- Arthralgia (pain in joint) ,etc
(III) Acute tubular necrosis :- There are 3 phases of ATN :-
# Oliguric phase :-
Function of tubular cells is reabsorption and secretion during urine formation.
In Oliguric phase, cell injury occurs,but it is not irreversible. There is loss of cell polarity and brush border.If the insulting factor is removed at this phase, complete recovery can occur.
Damage to tubules disrupts the process of urine formation and results in Oliguria.
Decreased urine output leads to fluid overload in the body resulting in conditions like
- ascites,
- pulmonary edema,
- pedal edema,
- raised JVP i.e jugular venous pressure (due to increased fluid in vessels).
Other symptoms in oilguric phase are - Azotemia (Elevated levels of urea and other nitrogen compounds in the blood.)
It occurs because kidney tubules have been damaged , and they're unable to get rid of nitrogen waste in our body.
- Hyperkalemia (due to direct injury of cells responsible for K+ secretion.)
# Maintainence phase:- glomerular filtration rate reaches its lowest point and urine output is at its lowest.
- irreversible renal parenchymal injury occurs.
# Recovery phase -
- both tubular cell death and cell regeneration occur simultaneously.
The balance between these 2 phenomena and the predominance of regeneration leads to recovery phase. There is structural and functional renal recovery with a restored GFR. During the recovery phase, apoptosis helps in the remodeling of the injured renal tubules.
- Initially, diuresis may occur due to delayed recovery of tubular cell function compared to increased glomerular filtration due to early repair of capillaries. Function of tubular reabsorption may not be fully developed yet thus causing diuresis.
This leads to
Polyuria
Dehydration
Hyponatremia due to loss of sodium
Hypokalemia due to loss of potassium
- Afterwards, the renal function and urine output normalises.
NOTE :- Not all the patients of ATN have Oliguric ARF , some patients have normal urine output ( when Injury to cells is less)
⭐⭐⭐⭐⭐⭐⭐⭐
(C) SYMPTOMS DUE TO POST RENAL CAUSES OF ARF:-
- Anuria ( <100 ml / day) due to obstruction to the flow of urine.
- Hematuria ( either due to trauma by stones ,etc or due to Infection and inflammation caused because of clogging of urine.)
- Difficulty in micturition
- Pain in loin and renal colic
( When the obstruction causes distension of bladder, ureter, or the kidney, it usually causes pain due to stimulation of the nerves in the walls . If the kidney is distended, renal colic can develop. Renal colic is an excruciating pain between the ribs and hip on the affected side that comes and goes every few minutes.)
⭐⭐⭐⭐⭐⭐⭐⭐
(D) Many of the cases of ARF show Uremia and fluid overload.
- Uremia can lead to
# Nausea and vomiting ( Urea triggers receptors in CTZ i.e vomiting centre)
# Anorexia
# Pruritus ( due to uraemia-related abnormalities involving calcium, phosphorus , accumulation of uraemic toxins, systemic inflammation )
# Uremic encephalopathy ( due to accumulation of toxins) - seizures, altered mental status, myoclonus
# Uremic pericarditis ( inflammation due to urea)
- Fluid overload may present as
# pulmonary oedema
# dyspnea
# ascites ,etc
6) INVESTIGATIONS OF ACUTE RENAL FAILURE :-
(I) Creatinine -
Blood urea & creatinine is increased
in Acute Renal Failure but creatinine
is not reliable because:
# Other factors may also influence:
Age, Sex, Nutrition, Hydration,
Muscle mass, etc.
# After 50℅ of renal failure
creatinine increases but not before
it.
(II) Other Markers - They detect ARF in
early stage :
# NGAL (Neutrophil Gelatinase Associated Lipocalin)
# KIM - 1 (Kidney Injury Molecule-1)
# IL-8.
# Cystatin C.
(III) Other biochemical abnormalities -
# Hyperkalemia - due to decreased
potassium excretion.
# Hyperphosphatemia - due to decreased
PO4 excretion.
# Hypocalcemia - As PO4 is
increased due to its decreased
excretion, it binds to Calcium ions
& Ca3(PO4 )2 deposits in bone
leading to decreased Calcium
concentration in blood.
# Hyperuricemia.
(IV) ECG - Changes due to hyperkalemia.
(V) Chest X-ray - Shows pulmonary
edema.
(VI) Abdominal X-ray & USG - Post renal
obstruction.
(VII) Kidney biopsy.
(VIII) Urine Microscopy -
# Glomerulonephritis - shows red
cell casts, proteinuria.
# Allergic tubular interstitial nephritis - shows WBC , RBCs, eosinophilia.
# Acute Tubular Necrosis - shows
epithelial cells, coarse granular
casts (Due to tubular injury
there is glycosuria, proteinuria
aminoaciduria)
7) MANAGEMENT OF ACUTE RENAL
FAILURE :-
(I) Treatment of cause.
(II) I.V. fluids for fluid & electrolyte
balance.
(III) Acidosis - bicarbonate (i.v./ oral)
(IV) Treatment of hyperkalemia (if it is
present)
(V) If severe pulmonary edema -
Do hemodialysis.
(VI) For drug induced allergic nephritis -
Stop the drug & give steriods.
(VII) Salt restrictions & daily protein
not more than 40 g/day.
(VIII) After fluid & electrolyte correction-
Daily fluid intake = Volume equal
to urine output
+
400 ml
(IX) If conservative method fails -
Do haemodialysis.





I wish u had made this last year 😅
ReplyDeleteAnyways keep it up 🤠
Thank you so much 😊😊
Deleteकौतुकास्पद लेखन👌👌 उत्तम
ReplyDeleteThank you so much 😊😊
Deleteअप्रतिम लिखान असच लिहीत राहा
ReplyDeleteThank you so much 😊😊
Delete👌👌 nice keep it up
ReplyDeleteThank you so much 😊😊
Deleteमस्त
ReplyDeleteThank you so much 😊😊
DeleteGood beta
ReplyDeleteThank you so much 😊😊
Delete👌👌
ReplyDeleteThank you so much 😊😊
DeleteVery good writing
ReplyDeleteThank you so much 😊😊
Deleteखुप छान बेटी👍☺️
ReplyDeleteThank you so much 😊😊
Deleteवेल डन
ReplyDeleteThank you so much 😊😊
DeleteVery nice
ReplyDeleteThank you so much 😊😊
DeleteGood writing
ReplyDeleteThank you so much 😊😊
DeleteSuperrrr
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteBahot acche
ReplyDeleteThank you so much 😊😊
DeleteHit
ReplyDeleteThank you so much 😊😊
DeleteVery well
ReplyDeleteThank you so much 😊😊
DeleteGreat job
ReplyDeleteThank you so much 😊😊
DeleteNicely written
ReplyDeleteThank you so much 😊😊
DeleteFabulous!
ReplyDeleteThank you so much 😊😊
DeleteGood
ReplyDeleteThank you 😊
DeleteExcellent
ReplyDeleteThank you so much 😊😊
DeleteNice
ReplyDeleteThank you so much 😊😊
DeleteVery good
ReplyDeleteThank you so much 😊😊
DeleteGreat
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteWriting very well. Keep it up beta
ReplyDeleteThank you so much for your appreciation 😊😌
Delete👌👌👌
ReplyDeleteNice work
ReplyDeleteThank you so much 😊😊
DeleteAlways keep writing👌
ReplyDeleteThank you so much 😊😊
DeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDeleteThank you so much 😊😊
ReplyDelete